Almost 40% COVID-19 patients have PE on CTPA
By Kate Madden Yee, AuntMinnie.com staff writer
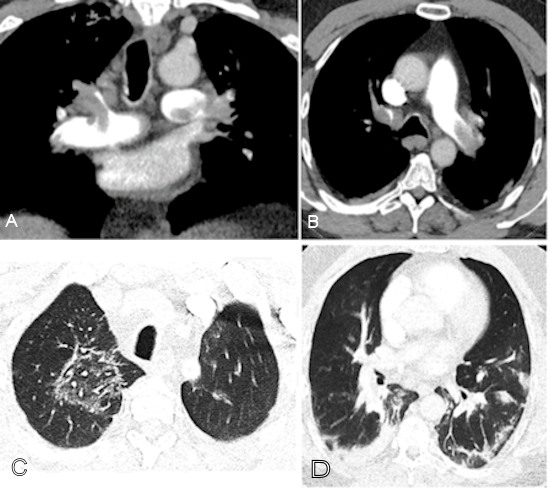
July 6, 2020 — Researchers have discovered that 37% of patients with confirmed COVID-19 disease are found to have a pulmonary embolism (PE) on CT pulmonary angiography (CTPA). Their results were published July 2 in Radiology: Cardiothoracic Imaging.
The study findings could help clinicians better apprehend the PE rate in patients with COVID-19 and manage their care, according to a team led by Dr. Mark Kaminetzky of NYU Langone Health in New York City.
“Understanding pulmonary embolism rate and contributing comorbid, clinical, laboratory, and imaging characteristics may aid in management of prothrombotic events in [COVID-19-positive] patients,” the group wrote.
As doctors have continued to deal with the COVID-19 pandemic, awareness of the disease’s manifestations has grown, particularly regarding the risk of PE. CTPA can be an effective tool for stratifying this risk, but in very ill COVID-19 patients, its pros and cons must be carefully evaluated.
“In particular, there is a heightened awareness of pulmonary embolism in [COVID-19-positive] patients, which would diminish the already compromised pulmonary function and capacity,” the group wrote. “Many acutely-ill and hospitalized [COVID-19-positive] patients have multiorgan failure and possibly acute kidney injury, and decisions as to whether CTPA is performed take into consideration both the potential risk of nephrotoxicity from intravenous contrast administration and the benefit of diagnosing pulmonary embolism.”
The team sought to investigate the prevalence of PE and the relationship to the condition and D-dimer levels as a way to decide whether CTPA would prove beneficial to COVID-19 patients. The study included 62 COVID-19-positive patients who underwent CTPA between March 13 and April 5 and 62 patients who underwent CTPA before the first local COVID-19 case was reported. The investigators noted patients’ comorbidities, lab findings, clinical outcomes, and presence of venous thrombosis.
Kaminetzky and colleagues found that 37.1% of COVID-19 positive patients had pulmonary embolism, a much higher rate than those patients in a control cohort who underwent CTPA but did not have the disease (14.5%).
The group also found that D-dimer levels assessed closest to the date of the CTPA exam were higher in patients with COVID-19 and PE, and the D-dimer levels correlated to a higher CT severity score: Mean D-dimer was 1,774 ng/mL D-dimer units (DDU) in patients with CTPAs negative for PE and 6,432 ng/mL DDU in patients with CTPAs positive for PE (p < 0.001).
“The heightened risk of pulmonary embolism in COVID-19 was supported by our elevated percentage of positive CTPA exams in [COVID-19-positive] patients, compared to the 22.7% and 30% rates reported in cohorts composed of only acutely ill intensive care unit patients prior to COVID-19,” the group wrote.
The study suggests a way to grade patients’ risk for pulmonary embolism — and thus make more accurate treatment and disease management decisions, the group concluded.
“PE can be a cause of decompensation in [COVID-19 disease], and D-dimer can be used to stratify patients regarding PE risk and severity,” it wrote.
