Subtraction CTA boosts in-stent restenosis evaluation
By Eric Barnes, AuntMinnie.com staff writer
January 9, 2015 — A new study of digital subtraction CT angiography (DSCTA) found that it vastly improved the visualization of the stent lumen by eliminating metallic artifacts, according to researchers from Japan. The technique was particularly effective in improving the assessment of very small stents.
Subtraction coronary CTA did a better job of visualizing the arterial lumen within metallic stents, and it also improved the evaluation of in-stent restenosis, the group reported last month at the RSNA 2014 meeting. More than 80% of stents 2.5 mm in diameter and larger can be evaluated using the technique, which also improved specificity and reduced the number of nonevaluable stents from 56 to four, the researchers found.
“Coronary metallic stents often interfere with the evaluation of in-stent restenosis; however, recently, subtraction coronary CT angiography has been introduced to overcome this problem,” said Dr. Makoto Amanuma from the radiology department of Takase Clinic in Takasaki, Japan.

Dr. Makoto Amanuma from Takase Clinic.
Digital subtraction CT angiography, like the conventional digital subtraction angiography (DSA) it is steadily replacing, works by subtracting precontrast from postcontrast-enhanced images to visualize anatomy in challenging environments where bone, soft tissue, or, in this case, metallic stents can create image artifacts.
The clinical feasibility of using DSCTA to detect in-stent restenosis and coronary artery calcification has been previously reported, Amanuma said. The present study aimed to assess the clinical usefulness of subtraction coronary CTA for evaluating restenosis of metallic coronary artery stents.
Beginning with 897 patients with metallic coronary stents, the researchers performed subtraction coronary CTA in 387 patients, and they also analyzed the results of 99 patients (mean age, 54 ± 6 years) who underwent both subtraction CTA and invasive coronary angiography.
All imaging was performed on a second-generation 320-detector-row CT scanner (Aquilion One Vision, Toshiba Medical Systems) following administration of IV contrast at 120 kV and 600 ± 193 mAs. The prospective one-beat scan protocol required a single breath-hold and acquired images in the middle of diastole, using adaptive iterative dose reduction (AIDR) 3D and full image reconstruction if the heart rate was 51 beats per minute or less. The target heart rate was 61 beats per minute, controlled by oral administration of beta-blockers.
The CT images were evaluated by a cardiologist and a radiologist, and a second cardiologist also evaluated the invasive coronary artery images. They reviewed both the conventional and DSA images, calculating diagnostic accuracy and analyzing factors that affected subtraction effectiveness, Amanuma said. The mean heart rate was 54 ± 6 beats per minute, and the mean total radiation dose was 6.7 mSv ± 4.2.
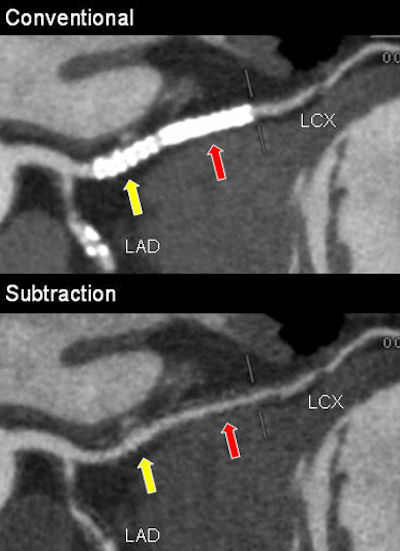
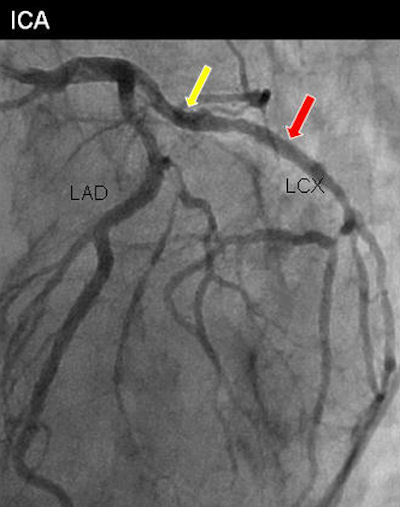
Top, 67-year-old man with two 3-mm stents placed in left circumflex (LCX) artery seen in conventional coronary CTA. Above, luminal patency became evident with subtraction. Below, patency is confirmed with invasive coronary angiography. All images courtesy of Dr. Makoto Amanuma.
There was a sharp improvement with the digital subtraction CTA protocol compared with conventional CTA, with invasive angiography as the gold standard. DSCTA scored higher in sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy, as indicated below.
| DSCTA vs. CTA for stent imaging | |||||
| Exam | Sensitivity | Specificity | PPV | NPV | Accuracy |
| Conventional CTA | 48.6% | 58.5% | 13.9% | 81.9% | 57.3% |
| DSCTA | 62.9% | 91.7% | 66.6% | 94.7% | 88.2% |
Fifty-six stents couldn’t be assessed before subtraction, compared with four after subtraction. Among the factors causing stent nonassessability, size was by far the most important, with smaller stents harder to assess.
Still, with the use of DSCTA, stent assessability improved from approximately 78% to 92% for 3.5-mm stents (p = 0.0503), from 61% to 90% for 3.0-mm stents (p = 0.0001), and from 37% to 81% for 2.5-mm stents (p = 0.0001).

Left, patient has one 2.5-mm stent and two 3-mm stents. Right, luminal patency became evident with subtraction for all three stents.
“For the larger stents, there was no statistically significant difference” in assessability with or without DSCTA, Amanuma said. However, for 2.5-mm stents, the improvement in assessability was more than 40 percentage points.
“DSCTA improved visualization of the stent lumen, resulting in improved diagnostic capabilities in the evaluation of in-stent restenosis, especially in terms of specificity, which is very important,” he said. “The frequency of restenosis is very small, so high specificity is important.”
Finally, using DSCTA improves assessability to more than 80% of 2.5-mm stents, an important advance “because 2.5-mm stents are now considered inappropriate for coronary CTA,” according to appropriateness criteria, Amanuma said. Careful heart rate control is critical to maintaining these results, he added.
