Less invasive, new approach to diagnose heart disease – Irish study
A clinical trial that saw high resolution scanning technology used to identify heart disease has been welcomed as a potential game-changer for cardiac treatment, being safe, minimally invasive and highly accurate.
A team at the University of Galway, in Ireland, used CT-scan imagery to pinpoint coronary artery disease and blockages as an alternative to traditional angiographs – an invasive procedure involving the puncturing of blood vessels, insertion of cables and use of dyes.
The Independent reports that the team, based at the university’s CORRIB Core Lab, analysed the images taken from patients in trial hospitals in the US and Europe.
The research was published in the European Heart Journal.
It found that the approach was 99.1% feasible, with the cardiac CT scanning offering good diagnostic accuracy without the need for invasive diagnostic catheterisation.
The trial was sponsored by the University of Galway and funded by GE Healthcare, based in Chicago, and HeartFlow, based in California.
Trial chairman Professor Patrick Serruys, established professor of interventional medicine and innovation at University of Galway, said: “The results of this trial have the potential to simplify the planning for patients undergoing heart bypass surgery.
“The trial and the central role played by the CORRIB Core Lab puts University of Galway on the front line of cardiovascular diagnosis, planning and treatment of coronary artery disease.”
The study involved 114 patients who had severe blockages in multiple vessels, limiting blood flow to their heart.
Serruys said the study offered the potential for a “monumental shift in healthcare”.
“Following the example of the surgeon, interventional cardiologists could similarly consider circumventing traditional invasive cineangiography and instead rely solely on CT scans for procedural planning,” he said.
“This approach not only alleviates the diagnostic burden in cath labs but also paves the way for transforming them into dedicated ‘interventional suites’ – ultimately enhancing patient workflows.”
A randomised trial involving more than 2 500 patients in 80 hospitals in Europe will now be undertaken.
Dr Yoshi Onuma, professor of interventional cardiology at University of Galway and the medical director of CORRIB Research Centre, said there were several benefits from the new approach.
“A catheterisation procedure is invasive and it is unpleasant for the patient,” he said. “It is also costly for the health service. While there is a minimal risk associated with the procedure, it is not entirely risk free.”
Commenting on the potential of the study, he added: “It may become a game-changer, altering the traditional relationship between GP, radiologist, cardiologist and cardio-thoracic surgeon for the benefit of the patient.”
Study details
Coronary bypass surgery guided by computed tomography in a low-risk population
Patrick Serruys, Shigetaka Kageyama, Yoshinobu Onuma et al.
Published in the European Heart Journal on 7 April 2024
Abstract
Background and aims
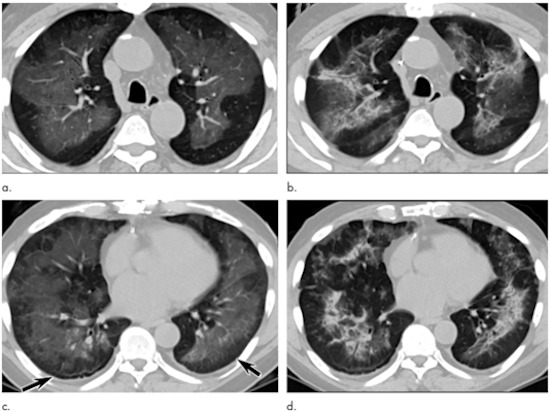
In patients with three-vessel disease and/or left main disease, selecting revascularisation strategy based on coronary computed tomography angiography (CCTA) has a high level of virtual agreement with treatment decisions based on invasive coronary angiography (ICA).
Methods
In this study, coronary artery bypass grafting (CABG) procedures were planned based on CCTA without knowledge of ICA. The CABG strategy was recommended by a central core laboratory assessing the anatomy and functionality of the coronary circulation. The primary feasibility endpoint was the percentage of operations performed without access to the ICA. The primary safety endpoint was graft patency on 30-day follow-up CCTA. Secondary endpoints included topographical adequacy of grafting, major adverse cardiac and cerebrovascular (MACCE), and major bleeding events at 30 days. The study was considered positive if the lower boundary of confidence intervals (CI) for feasibility was ≥75% (NCT04142021).
Results
The study enrolled 114 patients with a mean (standard deviation) anatomical SYNTAX score and Society of Thoracic Surgery score of 43.6 (15.3) and 0.81 (0.63), respectively. Unblinding ICA was required in one case yielding a feasibility of 99.1% (95% CI 95.2%–100%). The concordance and agreement in revascularization planning between the ICA- and CCTA-Heart Teams was 82.9% with a moderate kappa of 0.58 (95% CI 0.50–0.66) and between the CCTA-Heart Team and actual treatment was 83.7% with a substantial kappa of 0.61 (95% CI 0.53–0.68). The 30-day follow-up CCTA in 102 patients (91.9%) showed an anastomosis patency rate of 92.6%, while MACCE was 7.2% and major bleeding 2.7%.
Conclusions
CABG guided by CCTA is feasible and has an acceptable safety profile in a selected population of complex coronary artery disease.