Imaging findings on chest CT help predict lung cancer SBRT outcome
By Kate Madden Yee, AuntMinnie.com staff writer
April 14, 2022 — Imaging findings on chest CT conducted before a patient undergoes stereotactic body radiation therapy (SBRT) for stage I lung cancer appear to help predict treatment outcome, according to a study published April 13 in the American Journal of Roentgenology.
Noncancerous chest CT findings such as higher coronary artery calcium (CAC) scores, higher pulmonary artery-to-aorta ratio, and lower thoracic skeletal muscle index all suggest worse overall survival, wrote a team led by Dr. Ismail Tahir of Massachusetts General Hospital in Boston. And this research result suggests that CT has an even more important role to play for predicting treatment outcomes.
“Given the universal availability of chest CT scans in patients with lung cancer, imaging phenotypes remain an underutilized resource that could aid prognostication and clinical decision-making,” the group noted.
SBRT is the standard of care for patients with early-stage non-small cell lung cancer. But predicting the outcome of this treatment can be tricky, the authors explained.
“Treating physicians rely on multiple factors including patient age, Eastern Cooperative Oncology Group (ECOG) performance status, and comorbidities when making decisions regarding patient management and follow-up,” they wrote. “Although clinical features provide important insight into patient characteristics, ECOG performance status is subjective, and patient chronological age may not reflect biological age or resilience to cancer treatment.”
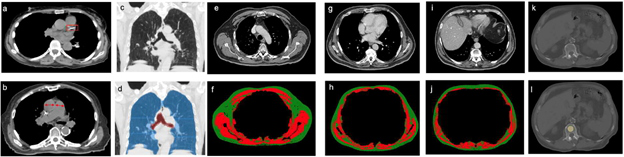
Tahir’s group conducted a study that included 282 patients with stage I lung cancer who were treated with SBRT between January 2009 and June 2017. Each patient underwent chest CT before beginning SBRT to measure their CAC score, pulmonary artery-to-aorta ratio, presence of emphysema, and body composition.
The authors found that CAC score, pulmonary artery-to-aorta ratio, and skeletal muscle index were all associated with poorer outcomes after SBRT for stage I lung cancer (p < 0.05); when the team added clinical factors to these imaging features, their model’s effectiveness improved even further at five years after treatment compared to using clinical factors alone. They measured the effectiveness of each metric based on area under the receiver operating curve (AUC) values.
| Ability of clinical and imaging characteristics to predict outcome after SBRT | |||
| Time (year after treatment) | Clinical characteristics alone | Imaging characteristics alone | Clinical and imaging characteristics |
| 1 year | 0.55 | 0.69 | 0.68 |
| 3 years | 0.61 | 0.67 | 0.67 |
| 5 years | 0.61 | 0.74 | 0.75 |
| 7 years | 0.73 | 0.73 | 0.79 |
| 9 years | 0.68 | 0.88 | 0.92 |
The study suggests that imaging markers may be more important than clinical variables when it comes to predicting overall survival in patients undergoing SBRT for early-stage lung cancer. But it would be a good idea to incorporate the two.
“Additional data are needed to externally validate our model toward establishment of a comprehensive prediction tool that incorporates [both] clinical and imaging features,” the investigators concluded.
